Enhancing Clinical Teaching: Top 10 Evidence-Informed Strategies for Faculty
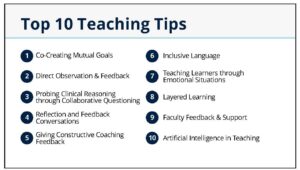
On October 16th, the UBC Division of Cardiology hosted an Educational Grand Rounds session led by Dr. Parvathy Nair and Dr. Heather Buckley, titled “Top 10 Teaching Tips”, offering faculty members practical, evidence-informed strategies to enrich their teaching practices in clinical settings. Drawing from their work with the Office of Faculty Development, the presenters emphasized the evolving nature of medical education and the importance of adapting teaching approaches to meet the needs of today’s learners.
- Co-Creating Mutual Goals
Teaching is no longer a one-way transmission of knowledge. Faculty are encouraged to engage learners in setting shared goals at the outset of a rotation or at the start of a scheduled week. This approach fosters alignment between learner interests and clinical realities. For example, if a resident is interested in heart failure management but the clinic primarily sees chest pain cases, a brief end-of-day discussion or targeted teaching moments can bridge the gap.
- Direct Observation & Feedback
Direct observation remains a cornerstone of effective clinical teaching. Faculty need not observe learner’s encounters—brief, focused observations can yield credible and actionable feedback. Clarifying whether feedback is formative or tied to an Entrustable Professional Activity (EPA) helps manage learner expectations and reduces performance anxiety.
- Probing Clinical Reasoning Through Collaborative Questioning
Questioning is a powerful teaching tool when used thoughtfully. Faculty should frame questions to explore the learner’s reasoning rather than test recall. Setting the stage for collaborative questioning, where learners understand the intent and feel safe to say “I don’t know”—creates a supportive learning environment. Try to understand what the learner knows, let them know you do not expect them to know everything. Be aware of the resident’s vulnerability when they express “I don’t know”, be supportive in your teaching.
- Reflection and Feedback Conversations
Start feedback conversations by inviting the learner’s perspective. While self-assessment may be imperfect, it provides insight into the learner’s mindset. Faculty should focus on specific behaviors, offer clear suggestions for improvement, and prompt learners to summarize their takeaways to ensure mutual understanding. Focus on what they did well, what they can improve upon, and what they should start doing next. Think about actions, what they are doing as opposed to characteristics or attributes that are not permeable.
- Giving Constructive Coaching Feedback
Constructive feedback should be timely, specific, and transparent. Faculty are encouraged to describe observed behaviors rather than infer intent, and to document goals for future reference. Offering learners a choice about when to receive feedback and involving program directors when needed can enhance receptivity and effectiveness. Invite learners to share their recollection of an observation or reasoning for their explanation. This can reveal knowledge gaps and learning opportunities for faculty.
- Inclusive Language
Inclusive language fosters respectful and welcoming learning environments. Faculty should avoid assumptions and use people-first language. For example, instead of saying “Go see the chest pain in room 2,” say “Please assess Mr. C in room 2, who is experiencing chest pain.” This shift acknowledges the person behind the diagnosis and promotes dignity in care. Avoid expressions that stereotype, stigmatize, or trivialize individuals or populations. The UBC Faculty Development office provides an inclusive language guide for your reference: Inclusive Language Guide.
We want to promote a safe and more open learning environment where people know that they can share themselves, not be dismissed, silenced, or looked down upon.
- Teaching Through Emotional Situations
Emotionally charged clinical events can deeply affect learners. Faculty should acknowledge the emotional impact, offer space for reflection, and model coping strategies. Determine and note a time available to engage the learner in a discussion about the event. Share coping strategies for emotionally charged situations with your learners.
Encourage learners to connect with their support system and ensure that the learner is able to continue clinical duties providing a compassionate timeline to return if necessary. Even brief check-ins after difficult cases can significantly support learner well-being and resilience.
- Layered Learning
Layered learning—where multiple levels of learners work together—can be highly effective when structured intentionally. Faculty should set expectations, support near-peer teaching, and involve patients when appropriate. We should set a culture of learning where trainees are not competing to provide a right answer, but we have a collaborative discussion by asking for elaboration from anyone in the team. Psychological safety and clear communication are key to successful team-based learning.
- Faculty Feedback & Support
Faculty benefit from receiving feedback from learners, but power dynamics can hinder open dialogue. Strategies such as asking learners for suggestions for future teaching or using “feedforward” techniques can facilitate constructive conversations. Ask your learners what did they find most helpful on your teaching week, or what did they enjoyed the most. Modeling a growth mindset encourages learners to engage meaningfully. Be honest about how much you value feedback from residents. Talk about how you applied feedback that you’ve received in the past. Encourage the resident to use the online feedback forms
- Artificial Intelligence in Teaching
Generative AI is increasingly present in clinical education. Faculty should guide learners in its ethical and effective use, emphasizing the importance of verifying outputs and maintaining patient confidentiality. AI can support administrative tasks but must not replace critical thinking. UBC is actively developing policies and resources to support faculty in navigating this evolving landscape.
These teaching tips reflect a commitment to learner-centered, inclusive, and adaptive education. Faculty are encouraged to integrate these strategies into their clinical teaching and to access further resources through the UBC Office of Faculty Development at fac.med.ubc.ca.
For questions or support, please contact fac.dev@ubc.ca.